Jodie Mills, RN works with CareFlight’s Top End Medical Retrieval Service, flying out of Darwin across vast stretches of the Northern Territory. She grew up in the Royal Melbourne Hospital ICU before moving to Darwin 8 years ago where she completed midwifery studies. She joined CareFlight 4 years ago and slightly pities all those who don’t get to fly in the top end.
When asked to contribute to a blog and write about psychiatric aeromedical retrieval all I heard was my colleagues’ collective signs of “not another psych job!!”
The thing is, I’ve developed a bit of an interest in these patients after closely looking at the psychiatric retrievals in NT for the last 3 years. This specialised patient group presents a huge challenge to both the flight crew and our remote colleagues when presenting acutely unwell in our communities.
By the Numbers
I recently presented at the ASA/FNA/ASAM Aeromedical Retrieval Conference in Brisbane. I thought maybe we had a few psychiatric patients but I quickly realised after my presentation that the number of psychiatric retrievals we undertake in the top end is well above average i.e. its extremely high (15% of our total missions).
From Feb 2012 to the 20th October 2014 we retrieved 651 psychiatric patients, averaging 22-24 per month – it’s an almost daily occurrence. Demographically the patient population remains consistent with approx. 90% of patients Indigenous Australians, with male to female ratio if 1.45:1. The mean age is 31, however our youngest was 12, our oldest being 74 years.
We have only intubated 3% of this population which has led to expedited admission to the singular psychiatric facility at Royal Darwin Hospital (RDH). The inpatient psychiatric ward at RDH has a catchment area of 700,000 square kilometres.
It’s Not Just a Local Thing
Mental illness throughout the world is on the increase with the WHO (2014) predicting mental illness to be second only to cardiovascular disease for burden of disease by 2030. The stigma associated with mental health issues remains the greatest obstacle to such patients accessing appropriate care. This stigma may be even more pronounced in remote Indigenous communities. Drug induced psychosis, predominantly cannabis (397 patients), followed by suicidal ideation/ hanging (224) were the most common diagnosis with the remaining patients having bipolar, mania or behavioural disturbances.
At the ASA conference I asked my aeromedical peers “How do you transport your psychiatric patients?” the answer was “we don’t, they go by road”. I quickly realised then that CareFlight and other retrieval services working in truly remote areas provide a unique service.

The Perfect Storm
We all know too well the challenges involved in the aeromedical transport of compliant patients who are unwell. However if we add delusions, hallucinations, physical aggression a tendency to physical violence and homicidal thoughts into the mix we have a potential aviation disaster on our hands. These are the just some of the symptoms the majority of our psychiatric patients display when referred to CareFlight. We then face the task of transporting such patients in a small aircraft where we will place seatbelts and wrist and ankle restraints on them, we will sit approximately 50cm away from them and the tell them they cannot smoke, they cannot go to the bathroom, they cannot eat or drink. I can’t imagine how stressful this must be for a patient that is already thought disordered.
What We Do
The biggest challenge for the aeromedical clinician is assessing the need and amount of sedation that will be required for safe retrieval of the acute psychiatric patient. If we have learnt anything it is definitely that “one-size DOES NOT fit all” when it comes to choosing sedative combinations to safely retrieve acute psychiatric patients. However we have found that pre-flight sedation with an atypical antipsychotic (olanzapine) and a sedative (diazepam) is of the utmost importance. As we become better skilled at treating psychiatric patients we have increased the pre-sedation (Olanzapine & Diazepam up to 20mg oral) which seems to be decreasing inflight sedation requirements. This enables the psychiatric patient to be admitted to the appropriate ward in a timely manner.
Top Tips for What to Do:
- Start sedation early:
As mentioned above, premedication prior to retrieval is vitally important. In most cases an antipsychotic (Olanzapine 10mg) and a benzodiazepine (Diazepam 10mg) is the premedication of choice. However, acute psychiatric patients presenting with drug induced psychosis (be it first or subsequent presentations) routinely require up to 20mg- 30mg of both Olanzapine and Diazepam orally. The first dose of sedation is given prior to the crew departing Darwin and then half an hour prior to the crews landing at the communities/ regional hospitals. This administration is overseen by the Medical Retrieval consultant (MRC) on duty. If the patient is not responding to the Olanzapine and Diazepam, the likelihood of requiring in-flight sedation is increased as is the probability of intubation for transport.
- In-Flight sedation:
We find in flight we tend to use midazolam, propofol and ketamine. The drug of choice is directly related to the flight doctor’s area of expertise. The ED Registrars tend to use midazolam and ketamine, whereas the ICU and Anaesthetic registrars head for the propofol and midazolam.
On arrival at the referral centre the patients are assessed for the need for further sedation prior to flight.
- Pre-Flight Sedation: Midazolam 2-5mg IV
- In-flight Sedation:
- Propofol Infusion 0.2-0.5mg/kg/hr and titrate as required
- Ketamine Infusion 0.5-1mg/kg/hr and titrate as required
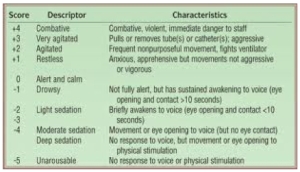
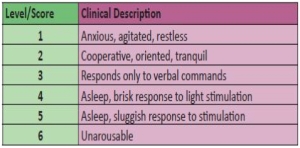
A Richmond Agitation Sedation Scale (RASS) of -3 (Moderate) to -4 (Deep) or a Ramsey Sedation score of 5 indicates the level of sedation required for safe transport.
The ability to discontinue the sedative and allow the patient to wake prior to admission at the receiving centre is extremely important. If the flight crew are able to deliver an acute psychiatric patient to the receiving centre awake and ready for assessment this expedites the patients’ admission to the in-patient facility from the emergency department or, optimally allows for direct entry into the inpatient facility at the receiving centre.
Richmond Agitation Sedation Scale:
Ramsey Sedation Scale:
- Managing the environment:
Managing the stressors of flight is extremely important when retrieving an acute psychiatric patient. Using ear plugs, blankets to keep patients warm, positioning for comfort when heavily sedated, limiting cabin conversation and ensuring physical restraint are fastened appropriately ensures the acute psychiatric patient does not experience any extraneous stressors throughout their flight.
- Local law enforcement:
On occasion the local law enforcement will be involved with the acute psychiatric retrieval. The resource poor environment of the community clinic necessitates the presence of police to help control patients as documented under the section 9.
- Coordination:
The coordinating Medical Retrieval Consultant will liaise with the Consultant Psychiatrist on call at the hospital, alerting them to the impending admission. The Consultant Psychiatrist then coordinates with their in-patient team to ensure timely assessment of the patient if they are to be admitted through the emergency department.
Although the collective groan when another psychiatric retrieval arises resonates through the base we remain steadfast in our support to our rural and remote colleagues and we will continue to play a vital role in maintaining safety of the community, the families and the patients who are all touched by mental illness in the top end of the NT.

Reblogged this on PHARM.
LikeLike
great post, Jodie. Keep up the good work at the Top End retrieval. Time to publish your results formally on ketamine!
LikeLiked by 1 person
Thanks very much Minh, publication in the works..watch this space
LikeLiked by 1 person
First up – thanks so much for making this available through “The Collective” – I firmly believe in the free sharing of appropriate (non-proprietary) information, in the spirit of sharing tacit knowledge and improving outcomes for all.
Secondly – great article on psych retrieval. At 15% of your case-mix, that is about the same disease burden as we see for trauma at MedSTAR (SA) ie : 15% of missions. The rest? Mostly medical IHTs. yet everyone get’s all excited about ‘sexy’ trauma and tends to ignore the mundane. Kudos on you for this work on psych transfer.
I like the link to RASS prompt cards; but I wonder if you’ve seen the psych risk asessment matrix that my mate Casey Parker of BroomeDocs came up with a few years back – trying to facilitate a sensible approach for rural doctors when weighing up the risks of sedation vs inherent airway risks for some punters. I will see if can dig it out…
LikeLike
We’ll let Jodie pitch in with her clinical thoughts but so glad we could share her insights.
First query – how much is “proprietary” in what we do? The common areas in care from different organisations are a lot bigger than the not common bits.
And nice point on the “sexy” vs mundane – do you think the medical emergency transfer would seem mundane to the patient? We’re betting not.
LikeLike
Ah-ha : here it is – from way back in 2011. Probably due an update! Whaddayareckon?
LikeLike
And really like the matrix approach. Would be interesting to see if Casey’s approach once he’s assessed the risk has changed.
LikeLike
Hi Tim,
Thanks for your comments. I agree that although acute psychiatric aeromedical retrieval may not be as topical as trauma, it is something we do (at times) nearly every day and as such complacency can be our undoing.
I hadn’t seen the Safe Sedation Matrix by Casey Parker but it looks like a great tool for rural and remote clinicians. I think a risk analysis involving acute psychiatric patients is an extremely tricky tool to invent (one that incorporates the spectrum of psychiatric illnesses). I like his colour coding approach and descriptions of each patient cohort. I think we can all imagine a black coded patient we have retrieved……challenging at the best of times.
LikeLike
Yes. Working in new paradigm now. A plan from A to Z for psych transfers
Of course ketamine is up there!
Will have to refresh it
Basic principle same – approach as any sedation / anaesthetic
LikeLike
Look forward to seeing the next edition Casey
LikeLike
Hi Jodie
great read- thanks for posting!
Interested that you have two different regimes – ketamine v propofol. It’s something I have wondered about, coming mainly from an anesthetic background and used to sedating everyone with Propofol infusions – but now working in an organisation where we use ketamine as our “agent of choice” for psychiatric transfers.
I would really be interested to know :
Do you find better outcomes with one regime over the other? Do patients under one wake up faster/better or are they similar?
Is your complication rate any higher with one over the other? I would expect propofol to have higher risk but with the experience of your medical staff, are complications in big groups minimised and similar? Or does the propofol group have a higher rate of complications/ poor outcomes?
Do you ever start one regime and find for any reason you swap over to the other?
Thanks for sharing your experiences
Patrick
LikeLike
* are complications in “both” groups minimised and similar? (Not big groups!)
LikeLike
Thanks Patrick,
As far as the difference between sedating with Propofol versus Ketamine….this is the next phase of our research and we will be able to answer that question with evidence. Personally, I find that Propofol induces more hypotension when utilised in an infusion but this could be anecdotal. I find boluses of Propofol are somewhat safer. I have not found any difference with the adverse reactions to PropofoI with any of our medical staff however as I’ve pointed out, different specialities favour different sedating regimes. We haven’t had any adverse effects from ketamine boluses or infusions at this point. As expected patients do wake up faster from Propofol but we are steadily becoming more adept at timing our cessation of ketamine for admission to hospital. We have not had an instance of emergence phenomenon to date, but this could be due to diligent premedication with benzo’s. There is definitely times when you get the patient who catches you out and it seems like you use an exorbitant amount of sedation however I find a combination of agents it that particular patient works well, however these are the patients who most likely require intubation due to our long flight times. If the patients are not moderately sedated (RASS -3 to -4) with premedication of a benzo and an anti-psychotic then the likelihood of that patient requiring intubation increases exponentially.
Again thankyou for your comments
Jodie
LikeLike
Thanks Jodie
I often wonder if the most effective sedation for our purposes would actually be a “ketofol” mix?
LikeLike
Yes I think ketafol would be a very interesting mix to try; it is always good to have options up your sleeve for the blacks
LikeLike
Hi Jodie, was reading your post earlier today whilst on retrieval shift and then had to go and do one! I think its great another aeromedical retrieval service is publishing this experience and work to look at alternatives to the traditional intubation and ventilation.
Like Patrick, I have wondered about the Propofol sedation and have been asked many times if its a reasonable option. I only knew of one case report out of MedSTAR in Adelaide of it being used, so a case series of it would be useful addition to the literature, thanks!
In many respects propofol should be the ideal agent, if not for the fact that many if not all patients needing evacuation are unfasted and many of the retrievals are not short duration.
thats why I still favour ketamine infusions. Our record that I want to see if you have exceeded is 4 hrs on a ketamine infusion at 500mg/hr. I know of an anecdotal case from WA of one case that went for 8 hrs on a ketamine infusion.
One thing I think we might be able to do is a multicentred trial of is nicotine patches during retrieval. I often have wondered if agitation on the flight is due to nicotine withdrawal and have last few years been putting nicotine patches on flights lasting more than 1 hr in known heavy smokers.
LikeLiked by 1 person
Hi Minh, we haven’t exceeded 4hrs on a Ketamine infusion at 500mg/hr, but I did read your article with Adam Pritchard (Sedation During Air Medical Retrieval of an Agitated Patient) with great interest. We are definitely finding that Ketamine is proving a valuable sedating agent for retrieval of acute psychiatric patients.
It would be interesting to see some evidence behind Propofol use in this patient group as I don’t think it can be discounted as a valuable adjunct to (or on its own) when sedating this patient group.
It would be great to do a multi-centred trial of nicotine patches during retrieval. My only experience with nicotine patches is in the ICU setting, but we found (anecdotally) that patients were less agitated throughout their admission with them applied.
LikeLike
NT & Qld multicentred retrieval trial !
About combining propofol and ketamine , we have tried that a few times . Not great results as often tended overshooting with the propofol . No clear advantage to midaz or droperidol + ketamine
I think ideally it should be delivered via propofol TCI pump system rather than manual titration then infusion
LikeLike
From top to bottom; Can we add SA to that trial?
In Mount Gambier (SA) we developed a 4 tiered pathway from therapeutic treatment to therapeutic sedation, with Ketamine last resort (Level 4) based on ketaminh’s article. We transfer about 40 a year and of these about 6% require L4 interventions. We adopted the Sedation Assessment Tool (SAT) from Newcastle, NSW, and put in 10 ancillary local work site instructions to support the pathway.
I approach this from a slightly different angle as a NP-MH who has had tremendous support from ED and MedSTAR in addressing this challenging area for our aeromedical teams, trying to make sure that when you arrive, things are as seamless as they can be.
Cheers
Leigh
LikeLike
Thanks Leigh, I definitely agree with Minh and yourself that we need to approach safe sedation of acute psychiatric patients from the ground up (there’s a pun I didn’t intend!!). We have found from preliminary studies that pre-medication at the referral site is of paramount importance and an essential conduit to safe aeromedical retrieval. The Remote Area Nurse’s and other clinic and hospital staff who attend to the treatment and cares of this patient group definitely make our job a whole lot easier…thankyou
And I definitely like the idea of a multi-centred retrieval trial…..
LikeLike
Hi Everyone,
One of my posts has been taken out of context and I have to apologise for not being more explanatory in my blog. When I wrote on the 7th January that Ketafol could be kept up your sleeve for the blacks: this was in relation to the SAFE Sedation Guide coding, it was not in a racial tone at all. I am sorry if others read this post as such.
Please see The SAFE Sedation Guideline (the Black Code is at the very bottom) below:
SAFE Sedation Guide
So here is how I reckon you should manage / sedate each of the groups (colours) in the SAFE Sedation matrix. Some of tis is not new – there are a few strategies that are not routine practice – let me know what you think:
WHITE: low-risk in both ways – if you are admitting these patients then you may need a sleeper, or mild anxiolysis only – easy, do your usual thing.
VIOLET: in this group I would advocate restraint, monotherapy, longer-acting agents and good nursing are all that is required.
INDIGO: Step away from the drug cabinet! You have little to gain from sedating a high-risk medical patient who is not too agitated. Good nurse care, orientation, reassurance and minimal stimulation are best – enlist family where possible
BLUE: This group need some sedation. The strategy I like with the healthy / thin patient is a decent dose of sedation – then see what happens – either you are good or you add a bit more – I like a combo of antipsychotic and benzo (eg, Olanzapine + Clonazepam). The mistake I see often is trying a little dose of x, then swapping to y, then z – suddenly the patient has subtherapeutic doses of 3 agents on board and it is hard to decide what to do next wen they don’t work!
GREEN: This group is the same management as BLUE – except you might want to do it in an environment where you can do airway stuff if needed whilst you are titrating. If you have time then titrate the sedation (something longer-acting), try and achieve fasting, maybe some metoclopramide and PPI for the reflux?
YELLOW: This group is tiger territory – their safety risk is either unknown or volatile – but you know they are likely to be an airway problem. I think here you should use non-pharmacological means first, try a small dose of shorter agent (eg midaz) and then a tincture of time. Two things might happen – either they settle and become “INDIGO” or they don’t – then you are looking at BLACK – see below.
ORANGE: This is the controversial bit. Thin, healthy, easy airway BUT very dangerous / violent punter – traditionally we have used big doses of all sorts to get them under control…. and then intubated them as there is no way the RFDS will fly this guy unless he in in a coma (quite sensibly). So my PROPOFOL as first line comes in here – why put the patient at risk with a day or two of heavy sedation / airway unprotected, urinary retention, staff being punched wen you can just jump in with what you are going to have to do eventually anyway? Sure talk to the RFDS team, arrange a transport, keep the Police in the department / handcuffs on etc until you are ready then – RSI, Propofol / fentanyl drip. Off to ICU for wake up then into a secure facility – minimise the risk to all parties.
RED: Same as ORANGE – but you might want to optimise your situation – await fasting if you can, have the best airway team you can get there. Keep the patient in the critical area / Resus bay with Police etc nearby. You might try a bit of sedation, but only if you are prepared to “go all the way” if the need arises
BLACK : “Damned if you do, damned if you don’t”. I am gonna post a case that falls into this category to illustrate the disasters that can occur in this area. Needless to say it ended very badly. My suggestion is to use the minimum drugs you can and have both a good airway setup / cric kit etc all there. DO not let the Police leave – handcuffs might be nasty but they are better than being dead. This is tough – there is no good answer – I will put up my case for comment soon. All I will say is I would rather be pulled up by the Mental Health Advocate legal team for being cruel with physical restraint of a live patient; than face the coroner about the sedation that resulted in the death of my patient….
LikeLike