You might recall a series more than a bit ago from Dr Alan Garner covering lots of thoughts on pelvic fractures and what might make sense for prehospital care. Well, he’s back at it with a case to get things rolling.
It is amazing what you find when you go looking.
Those who are regular readers of the CareFlight Collective will be aware of my concerns about the use of pelvic binders in lateral compression (LC) type fractures. You can find parts 1, 2, 3 and 4 here. In short a binder in the context of a LC fracture replicates the force vector that caused the injury and may make fracture displacement worse. There is evidence of this in both cadaver models and in real live trauma patients. However blind use of binders without knowing the fracture type (and even where it is known to be LC) has been considered safe as there were no reports that patients had deteriorated after application – until now.
Last year one of our teams applied a binder to a haemodynamically stable patient with a LC fracture. There was immediate haemodynamic deterioration and new leg length discrepancy which had not been present prior to application of the binder. The case report has been accepted for publication by the Air Medical Journal and about now would be a good time to say thanks to our co-authors from Westmead Hospital, Jeremy Hsu and Anne Douglas. You can find a copy of the accepted manuscript accepted manuscript here. You need to go and have a read of the manuscript then come back for the following comments to make sense so I suggest you do that now.
Go on…
I can wait …
Continuing…
Now that you have read the case report you can appreciate that this incident caused us considerable angst. We knew this was theoretically possible but it was still a shock when it actually happened. It has caused us to review our practice around binders to try and find the safest approach.
But at the same time we need to acknowledge that we live in a space of considerable uncertainty because we don’t have radiographs to guide our management in prehospital care. All we have is our reading of the mechanism (which is often pretty unclear), the clinical state of the patient and perhaps a finding of pubic symphysis diastasis on ultrasound to guide us. We have to acknowledge that we are going to get this wrong a reasonable proportion of the time.
So here is our reasoning and the place we ended up.
Firstly we need to remember that there is still no study of any kind (RCT or cohort) that has shown a statistically significant improvement in survival with binders. There is some suggestive case series data (mostly in anterior compression or “open book” fracture types) and the benefit observed is raised BP and possibly blood product usage, not survival. That is it. As it seems we can definitely cause harm, it is worth keeping in mind just how poor the evidence for benefit is as we work our way through the approach to binder application. One of my very experienced colleagues refers to binders as “pelvic warmers” due to the almost complete lack of evidence of benefit and I can’t tell him he is wrong.
First…
The first thing to consider is the stability of the patient. Placing binders in stable patients with a possible mechanism has been considered acceptable practice despite the theoretical risks and indeed it is the policy of our local Ambulance service in NSW to do exactly that.
Other services such as Queensland have a more conservative approach. They position the binder if there is a suggestive mechanism but only tighten it if the patient is unstable or becomes so. Given that there is absolutely zero evidence that haemorrhage has ever been prevented by placing a binder I think the Queensland approach is a good one. I know that there are reports of binders reducing fractures so perfectly that they have been hard to identify on subsequent imaging and it is impossible to say whether they would have bled without the binder, but benefit from prophylactic use has not even been investigated let alone proven. And since we have now demonstrated that you can take a stable patient and turn them into an unstable one the summary of the published evidence now is:
- Harm from binder application in stable patients = 1
- Benefit from binder application in stable patients = 0
I acknowledge that prevention of haemorrhage is fundamentally difficult to prove but we have decided to join the Queenslanders. We will position it in stable patients if we are suspicious but it is only tightened if and when the patient becomes unstable. First do no harm. If they are haemodynamically stable you can’t make things better, but you can makes things a whole lot worse.
Second…
Our next consideration as per the previous posts parts 1-4 is the mechanism. If it is clearly a lateral compression fracture then there is not even a biologically plausible way a binder can help. If you are doing an interfacility transfer, you have an Xray and it is a LC fracture, do not apply a binder no matter how haemodynamically unstable the patient is. Every reported case who has had a rise in BP associated with a binder has had either anteroposterior compression (the majority of cases) or a vertical shear injury. Therefore the evidence base for lateral compression fracture so far is:
- Harm from binder application in patients with LC injury = 1
- Benefit from binder application in patients with LC injury = 0.
Just don’t do it.
Now of course prehospital it can be really hard to know what the fracture type is. But there are occasions where it can only be a lateral compression such as in MVAs where the impact is directly into the patient’s door with intrusion against their pelvis laterally. Here is an example repeated from part 3:

In this case the car has slid into the pole sideways. The impact is directly into the driver’s door who has been pushed across the cabin partially onto the passenger seat breaking the centre console in the process. This can only be a lateral compression fracture and that is indeed what was found on pelvic plain film in the ED. We no longer put binders on these patients, no matter how unstable they are – the binder has no plausible mechanism by which it can improve things.
Third…
The last part of the equation for us was the policy of application by the local Ambulance service which I have already mentioned. We often turn up to find that a binder has already been applied. Should we take it off again if stable? If unstable and it really looks like a lateral compression injury? The damage if any has probably already been done. We are operating in an evidence free zone here of course. Our consensus of opinion was that if it was properly applied we should just leave it there.
So we derived an algorithm which works through these steps in the reverse order that I have discussed them as that is the workflow in the real world:
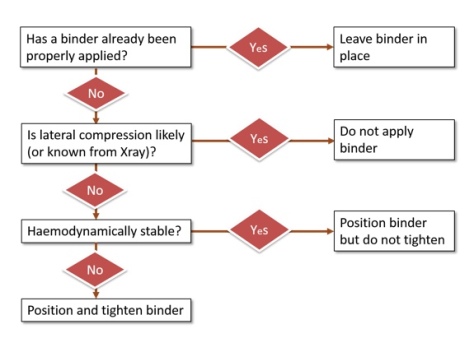
So the only patients who get a binder placed and tightened are the unstable patients where lateral compression is not likely from what we can see of the mechanism or we just don’t know the mechanism. If you re-read part 3 this is the group we are suggesting that ultrasound may help in the decision making. Benefit (in terms of improved BP, not survival) has only been demonstrated in patients with a widened symphysis so perhaps this is your single best clue that you have identified a patient who is likely to benefit from the intervention – if such a group actually exists.
The Wrap
The belief that pelvic binders are a benign intervention is becoming widespread even though there are already reports of serious complications such as massive necrosis from pressure injury (have a look here). No intervention helps all patients, and all interventions carry risk. The key is identifying the patients where the benefit outweighs the risk. Given that proof of benefit from binders does not yet exist, think very carefully about the risk that you could make things worse by tightening it and converting a stable patient into an unstable one. Use it only where the possibility of benefit outweighs the risk and there is just no possibility of benefit in a known lateral compression injury. It can therefore never be justified if you know that is the injury type. Similarly there is zero evidence of any kind for prophylactic use in stable patients, just a theory and even the theory does not make sense in lateral compression.
I find it difficult to believe that this is the first time a patient has deteriorated with a binder – we are just the first group to report it because we have been looking. Complications are typically poorly reported in prehospital care for a number of cultural reasons (see Davis’ classic work on prehospital intubation where significant complications were picked up only by examining the monitor output; it was not reported by the clinicians). Perhaps the temporal relationship between the binder and deterioration is not as clear as in this case, or the patient is already unstable and it is not possible to differentiate the additional bleeding caused by the binder from the bleeding that was already happening. Or the subsequent instability is not attributed to the binder by the caregivers who think “just as well we put the binder on” without realising they actually caused it.
We would be really interested to hear if anyone else has observed this too. But you won’t notice if you don’t look. In the meantime I think we all need to examine our practices to ensure that are only applying the devices where there is a possibility that the patient will benefit from this as yet unproven intervention. If there is no possibility of benefit, just don’t do it.
Notes:
You could always start with public cases like this to reflect on what we could do differently with pelvic binders.
Here’s the thing on the pressure necrosis with a pelvic binder again:
And if you’re interested in the stuff on this site you can always find the spot on this page to get your email in there


…And Alan hasn’t even mentioned the cost to healthcare – at around $100 per binder, the cost of indiscriminate, non-evidence based used is going to be huge.
LikeLike
Hi,
Interesting article.
Can I ask a couple of questions?
How do you apply the binder? Do you roll the patient? Is it possible that rolling the patient rather than the binder itself could have caused the fracture displacement?
Secondly what is you protocol for how tight the binder should be?Personally, I think we should be aiming to tighten the binder until we believe we have achieved anatomical reduction, if there is obvious worsening of the fracture or pain then the binder should be released until the pelvis looks anatomical. There is a tendency, particularly with ‘tension limited’ binders, to crank the binder ’til the buckle clicks rather than adjusting tension to what appears clinically appropriate.
I’ve seen a case of over tightening of a binder causing the fracture to appear clinically worse however the same fracture subsequently became severely displaced laterally when the binder was removed completely in hospital.
As always blanket rules are best avoided and you have to be guided by the clinical response you see in the particular patient in front of you at the time.
JS.
LikeLike
Thanks JS for opening a whole new can of worms! This topic alone could be number 6 in the series.
I don’t know how you tell when enough compression has been applied in the AP fracture types where I think a binder is probably of benefit when you don’t have imaging to guide you. As you note you tighten till “you believe”. I have no more to add as I don’t know of any real endpoint that we can use at the moment we pull it tight.
One of the manufacturers does have the tension limiting system and I hope that company does not use this case report as a marketing tool claiming it could not happen with their device. As you note, this might actually lead to too much tension. But how much is enough? There is a tiny bit of cadaver model evidence only as far as I am aware. Pretty keen to hear some thoughts on this.
Alan
PS we don’t apply the device by log rolling in our system, we slide it up or down into position depending on what is easiest in that patient or in the extrication scenario have it on the stretcher ready to go.
LikeLike
Great thought provoking stuff. I like the algorithm although it raises one question for me:
Can you please clarify – if you have a haemodynamically ‘stable’ patient with mechanism and clinical signs of an AP compression fracture (symphyseal widening, externally rotated feet, etc) would you wait for haemodynamic deterioration before tightening the binder?
Cheers
Cliff
LikeLike
Good question
Evidence free zone in a stable patient and weak evidence it might help if unstable. If you follow the Qld Ambulance protocol this patient if stable would not get the binder tightened unless they deteriorated. Given the evidence base as it stands this is reasonable and yes this is how our algorithm stands too. I agree the chance of doing harm in this circumstance is lower but I wonder how many patients would have those kinds of signs and be stable?
You could expand the algorithm for stable patients with a question about likelihood of AP compression injury and tighten where evidence suggested that injury type. This would also be reasonable but complicates the algorithm. There is no right or wrong answer as there is no actual evidence either way.
Alan
LikeLike