This is part 2 in Dr Alan Garner’s series on pelvic fractures and the approach to binders. You can find part 1 here.
In part one we had a look at the evidence for benefit from pelvic binders. In short there is no study yet published showing a significant improvement in mortality. Not even a cohort study.
Of course, it still might be OK to use them if they possibly help as long as there is no evidence of harm either (and they don’t cost too much). The probability of good has to outweigh the probability of evil. It is the potential for evil that I want to examine now so we can see where the balance lies.
Before we can do that though we need to have a quick look at the types of pelvic ring fractures (no one is suggesting that non-pelvic ring fractures of the pelvis benefit from a binder). So sorry folks but we have a bit of theory to re-visit.
Forces Down There
I use the Young and Burgess classification system as it is based on the force vector that caused the injury. In the prehospital world mechanism of injury is almost the only guide to injury type that is available to us (ultrasound may also give us some clues but we will talk about that in part 3).
AP compression injuries
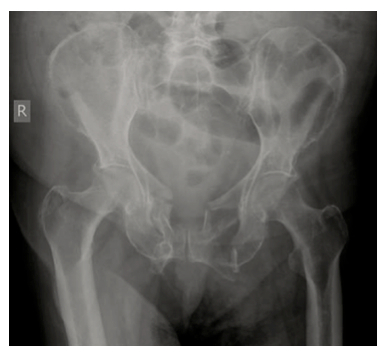
This is an anteroposterior (AP) compression injury. This is the kind of fracture you see in frontal motor vehicle collisions, commonly in motor bike riders, and people who have been crushed by a vehicle rolling over their pelvis for example. The hallmark is pubic diastasis with or without disruption of the SI joints. The AP compression causes the pelvis to open: one or both hemipelves undergo external rotation.
External rotation of the hemipelvis results in an increase in the volume of the pelvic cavity which then allows more pelvic haemorrhage to occur before the osseous and soft-tissue structures cause tamponade. Exsanguination is the primary risk & reduction of the increased pelvic volume is one of the goals of prehospital care.
When I was a boy Master taught me the way to reduce a fracture is to reverse the force that caused it in the first place. With this type of injury a pelvic binder makes biomechanical sense because it reverses the direction of the force which caused it. In severe AP compression injuries one or both hemipelves have been rotated backward. Applying a binder will rotate the hemipelves back towards each other, or “close the book”.
As I mentioned in part 1 there is very little evidence on whether this is actually helpful despite the theoretical benefit. Tan’s study was observational and involved only 15 subjects in an emergency department setting. All subjects had been X-rayed prior to application of the device so the type of injury was known (unlike our context in most cases). Nine of the 15 patients in this study had AP compression type injuries with wide diastasis of the pubic symphysis. Although there is some missing data, all patients with this pattern either had no change in MAP or it improved. So far so good.
There is a similar English study with 3 severe AP compression injury patients who improved with a binder (Nunn) but numbers are obviously pretty small.
Croce’s study appears to have had mostly AP compression fracture types (186 patients with breakdown between types not stated). Decreased transfusion requirements were found in the binder group at 24 and 48 hours (significant), the patients had decreased length of stay (significant), and lower mortality (non-significant). This does provide some support for use in severe AP compression injuries noting the methodology issues which I discussed in Part 1 with a retrospective study that included patients over a 10 year period.
There are a number of other studies which show improved alignment +/- blood pressure rise in AP compression type fractures in trauma patients, in cadavers and even in one prehospital study. None of these studies assess patient outcome though (I acknowledge this is difficult in cadaver studies!) Reduction can be so good that the fracture is difficult to see on subsequent Xray.
So in AP compression injury all the evidence points to better anatomical alignment, higher blood pressure, lower transfusion requirements, and shorter length of hospital stay when you use a binder. Mortality might be better too, but this remains to be proven. The important thing is there are no reports of adverse events in this group. When you see this fracture type on Xray or the mechanism suggests this injury – go for the binder. The risk of adverse advents is certainly outweighed by the possible benefits based on the best current evidence.
Lateral compression injuries
Lateral compression injury results in internal rotation of the affected hemipelvis. This internal rotation decreases rather than increases the pelvic volume so they tend to bleed less than the other types. Life threatening haemorrhage is still possible though. The hallmarks include sacral buckle fractures and horizontal pubic rami fractures.
Remember my boyhood teaching – “Grasshopper, to reduce fracture you must reverse force that caused it”. There is an obvious problem here as applying a binder replicates the causal force and if anything is likely to make it worse.
Have a look at this Xray of a lateral compression injury. Put a binder around the greater trochanters and pull. Are you a force for good or evil?
So what is the evidence? The Tan paper did not include any lateral compression injuries – remember that they had looked at the X-ray prior to application. I assume they looked and thought “well that is not going to help”. There is no evidence the Croce study included any either.
Is there evidence that a lateral compression fracture can get worse with a binder? (You have to be suspicious when binder studies appear to have avoided this fracture type altogether).
A recent Australian study (Toth) from 2012 had 8 cases with lateral compression that had binders applied. In three it resulted in increased pelvic deformity on subsequent Xray. They did not report the haemodynamic consequences. In the other 5 there was no improvement. There is biomechanical evidence of this in cadavers too e.g. Bottlang et al (if you look at this paper note again that they did not even attempt it in the LC3 injuries – the most severe grade).
Now this really disturbs me. There are docs I have met who are adamant that pelvic fracture patients should not be logrolled & should only be moved on scoop stretchers etc because the fracture fragments might move just with this limited motion. These same docs are however happy to put a binder on regardless of mechanism and pull, creating a much larger force than a logroll does, when we have direct evidence that binders increase fragment displacement in lateral compression injuries. Some consistency would be nice.
The bottom line is that there is no theoretical reason to believe that binders help in lateral compression injuries and lots of reasons to think they might make things worse. There is direct evidence in real world trauma patients that increased deformity of the pelvis does occur. There is no published data at all on the haemodynamic consequences when this happens, but I am betting you are not going to see improvement. The balance of risk here is on the dark side, not the light.
Bottom line is leave the binder in the bag in the bag for clear lateral compression mechanisms. It cannot help and there is published evidence of harm.
(Stay tuned for part 3 where we’ll get to vertical shear injuries – and other stuff).
References:





Thought provoking post reflecting important questions about binders, but my thoughts as a pelvic orthopaedic trauma surgeon:
Without imaging, pre-hospital identification of pattern is guesswork at best—in a shocked patient I’m not sure I would trust guesswork. The bleeding is caused by dissipation of energy orders of magnitude greater than can be generated by application of a binder which is unlikely to create further injury if applied firmly but carefully.
For me, the purpose of the binder is to keep the pelvis (and hence clot) still rather than reduction per se.There is good evidence that tamponade is not achieved simply by reduction because the disruption of fascial planes allows haematoma to escape from even a perfectly reduced pelvic ring. In a shocked patient applying a binder early is a single manouevre that reduces potential movement and can help preserve clot until diagnostic imaging can help decide whether other haemorrhage control or skeletal stabilisation is required. Springing the pelvis or a log roll are not single manouevres—they involve back and forth movement and would logically seem more likely to disrupt clot than a binder applied as early as possible (preferably before the clot has even started to form and certainly before coagulopathy).
Having said that I firmly believe binders should be removed as soon as possible especially in lateral compression injuries i.e. when it is clear that no stabilisation is needed (no active bleeding, or stable pelvis) or that it needs to be replaced with something more definitive. In lateral compression injuries the deformity is increased by the binder but in my experience this corrects spontaneously as soon as the binder is removed in the majority of cases, presumably because the weight of the legs tends to externally rotate the hemipelves and intra-abdominal pressure tends to “re-inflate” the pelvis. If left in place for too long it is conceivable that the position might become “sticky” not to mention the potential pressure area problems beneath the binder.
LikeLike
Thanks for getting involved Julian (and sorry it took a while to get to this today). Looking forward to posting the last bit of Alan’s thoughts soon.
A question that springs to mind:
– Keeping things still sounds good but would there be additional risk of bleeding with keeping it still in a more disrupted position in the setting of a lateral compression fracture? If you’ve induced a worsened position, will it potentially take longer to allow clot etc.?
On reading Alan’s thoughts, a couple of other scenarios come to mind. So often the force vectors won’t be crystal clear from the mechanism, or may be “mixed”. If you place a binder and see a worsening of haemodynamics, you could make an argument for releasing the binder. What about the patient where you place and they just don’t improve at all (particularly where you can’t find other sources of blood loss)? How do you assess whether you’ve contributed to a worsening bleeding situation (or can you even do that)?
Also, have seen cases where patient has a potential mechanism for lateral compression fracture (or even other fractures) and a binder is placed almost prophylactically. Thoughts on that?
LikeLike
Thanks and apologies for the delay in this reply! This discussion has crystallised some of my own thoughts and it’s nice to have the opportunity
I don’t think the position will make any difference to the likelihood of clot formation. In a lateral compression injury (LC) I find it difficult to imagine how the position, even if overreduced with a binder, could somehow “hold a vessel open”. As I alluded to before, the energy of the injury is where the vessel damage comes from, and applying a binder in a controlled fashion should not cause additional injury.
In any type of pelvic injury. the bleeding will be either:
1. Venous or bone ends: in which case keeping things still with a binder is likely to allow clot formation (low pressure bleeding, low or high flow).
2. “Slow” arterial (the sort of thing seen as a blush on contrast CT) which will probably trickle on even with a binder but at a rate which is compatible with survival to hospital and (ideally) interventional radiology if they don’t stabilise spontaneously (high pressure, low flow bleeding).
3. “Fast” arterial (e.g. free iliac rupture) which is likely to be fatal whatever one does, binder or not (high pressure, high flow bleeding).
This third group and high flow venous bleeders might represent the patients you refer to where there is no response. A binder isn’t likely to make much difference but I would still place one. These in extremis patients need rapid surgical intervention (surgical tamponade by packing) if they are to survive. Packing is only effective against a stabilised pelvic ring—a well placed (i.e. not too high) binder can achieve this stabilisation and can be replaced with something safer and more durable (usually an ex-fix) once control has been achieved.
The first two groups are self-selecting in reaching hospital and inevitably there will also be some venous haemorrhage associated with the “slow” arterial group so on balance a binder keeping the pelvis and clot still is likely to more of a help than a problem.
One potential issue with binder application in LC injuries might be occlusion of a major vessel by an over-reduced fragment pressing on it. As with any therepaeutic manouevre on a limb it would be best to assess distal pulses (if palpable) before and after binder application and consider release if occlusion appears to have occurred.
We have also seen use of binders increase “prophylactically” so that they can appear almost as ubiquitously as cervical collars in blunt trauma victims. No doubt far, far more binders are applied than are strictly necessary—by contrast in the past when resus room ex-fixes were recommended probaly too few of those were done. Where is the happy medium? Who knows, but binders tick many of the right boxes: easy to apply with little training; non-invasive; easy to carry in the pre-hospital environment and unlikely to cause much harm if removed/replaced in good time.
LikeLike
Reblogged this on PHARM.
LikeLike
Indeed
LikeLike
Thanks Julian for the comments.
Part of the answer is wait for part 3! Well, not the answer really, as there is so little decent evidence that much of this is speculation. There is reasonable observational evidence of course that reduction with a binder of really open AP compression injury results in improved haemodynamics. Does it stop bleeding? As you note probably not, at least not entirely. After the MAST suit experience I am really hoping improved haemodynamics this time is a good thing given that the bleeding is ongoing!
We are assuming that less movement is probably a good thing although again we have no direct evidence that it helps. Seems entirely reasonable though. I do note this recent paper that looked at the amount of movement in OTA type 61-C1 fractures in cadavers depending on where you placed a T-POD when the patient was log rolled, transferred between beds etc.
Does application position of the T-POD affect stability of pelvic fractures? Prasarn ML, Small J, Conrad B, Horodyski N, Horodyski M, Rechtine GR. J Orthop Trauma. 2013 May;27(5):262-6. doi: 10.1097/BOT.0b013e31826913d6.
http://www.ncbi.nlm.nih.gov/pubmed/22810548
Applying it around the trochanters as per Bottlangs original cadaver study did seem to produce less movement than around the ASIS. So we at least have some evidence that the T-POD does reduce fracture movement when applied optimally. Notably this was in Tile C1 injuries, which is the group where all the evidence points to probable benefit and I am certainly pretty keen to get a binder on in these patients. No one ever seems to study the lateral compressions!
I know that the lateral compression injuries are less likley to significantly bleed although it does still occur. I note your comments about the lateral compression injuries “re-inflating” when the binder is removed. The logical issue I have here is that we may induce clot disrupting movement when we apply the binder, and then it moves back again, potentially again disrupting clot when the binder is later removed. I just cant get my head around the idea that “in, out, in, out, shake it all about” is not going to be bad! Sorry, probably being a bit flippant but you get the idea.
Anyway part 3 which we should get posted in a week or so gives my theories on how we can perhaps be a little more selective in application while we get some real data to guide our decision making. Prehospital care to me seems one part evidence, one part art and three parts speculation at the best of times. We all really want to help patients and part of that includes being really vigilant that we are not actually doing harm.
LikeLike
Thanks. I take your point about limited evidence: there is very little to go on except intuition, common sense and experience.
To be clear about the pelvis re-inflating, I wouldn’t suggest removing the binder until it is clear that there is no active haemorrhage. Personally, I would look at the lactate, the presence or absence of a blush on contrast CT, the size of haematoma on CT as well as the clinical condition of the patient to help decide on whether there is active bleeding. In difficult borderline cases we have performed an interval CT to help guide decision making on binder removal/the next step in haemorrhage control. My personal opinion (disclaimer: based on surgical intuition) is that a decision should be made on binder retention, or replacement with ex-fix/internal fixation within 6 hours. This is primarily because of my concern over pressure areas under the binders. I know other surgeons are content to keep binders for up to 24 hours or possibly longer.
Once happy that there is no active bleeding the concerns over removal are minimised in LC fractures and the pelvis can be allowed to “re-inflate” after careful removal of the binder. In our unit it is the policy to perform further (usually plain) imaging after binder removal in all types.
A very interesting issue. I look forward to part 3.
Julian
LikeLike