Jodie Mills, RN works with CareFlight’s Top End Medical Retrieval Service, flying out of Darwin across vast stretches of the Northern Territory. She grew up in the Royal Melbourne Hospital ICU before moving to Darwin 8 years ago where she completed midwifery studies. She joined CareFlight 4 years ago and slightly pities all those who don’t get to fly in the top end.
When asked to contribute to a blog and write about psychiatric aeromedical retrieval all I heard was my colleagues’ collective signs of “not another psych job!!”
The thing is, I’ve developed a bit of an interest in these patients after closely looking at the psychiatric retrievals in NT for the last 3 years. This specialised patient group presents a huge challenge to both the flight crew and our remote colleagues when presenting acutely unwell in our communities.
By the Numbers
I recently presented at the ASA/FNA/ASAM Aeromedical Retrieval Conference in Brisbane. I thought maybe we had a few psychiatric patients but I quickly realised after my presentation that the number of psychiatric retrievals we undertake in the top end is well above average i.e. its extremely high (15% of our total missions).
From Feb 2012 to the 20th October 2014 we retrieved 651 psychiatric patients, averaging 22-24 per month – it’s an almost daily occurrence. Demographically the patient population remains consistent with approx. 90% of patients Indigenous Australians, with male to female ratio if 1.45:1. The mean age is 31, however our youngest was 12, our oldest being 74 years.
We have only intubated 3% of this population which has led to expedited admission to the singular psychiatric facility at Royal Darwin Hospital (RDH). The inpatient psychiatric ward at RDH has a catchment area of 700,000 square kilometres.
It’s Not Just a Local Thing
Mental illness throughout the world is on the increase with the WHO (2014) predicting mental illness to be second only to cardiovascular disease for burden of disease by 2030. The stigma associated with mental health issues remains the greatest obstacle to such patients accessing appropriate care. This stigma may be even more pronounced in remote Indigenous communities. Drug induced psychosis, predominantly cannabis (397 patients), followed by suicidal ideation/ hanging (224) were the most common diagnosis with the remaining patients having bipolar, mania or behavioural disturbances.
At the ASA conference I asked my aeromedical peers “How do you transport your psychiatric patients?” the answer was “we don’t, they go by road”. I quickly realised then that CareFlight and other retrieval services working in truly remote areas provide a unique service.

The Perfect Storm
We all know too well the challenges involved in the aeromedical transport of compliant patients who are unwell. However if we add delusions, hallucinations, physical aggression a tendency to physical violence and homicidal thoughts into the mix we have a potential aviation disaster on our hands. These are the just some of the symptoms the majority of our psychiatric patients display when referred to CareFlight. We then face the task of transporting such patients in a small aircraft where we will place seatbelts and wrist and ankle restraints on them, we will sit approximately 50cm away from them and the tell them they cannot smoke, they cannot go to the bathroom, they cannot eat or drink. I can’t imagine how stressful this must be for a patient that is already thought disordered.
What We Do
The biggest challenge for the aeromedical clinician is assessing the need and amount of sedation that will be required for safe retrieval of the acute psychiatric patient. If we have learnt anything it is definitely that “one-size DOES NOT fit all” when it comes to choosing sedative combinations to safely retrieve acute psychiatric patients. However we have found that pre-flight sedation with an atypical antipsychotic (olanzapine) and a sedative (diazepam) is of the utmost importance. As we become better skilled at treating psychiatric patients we have increased the pre-sedation (Olanzapine & Diazepam up to 20mg oral) which seems to be decreasing inflight sedation requirements. This enables the psychiatric patient to be admitted to the appropriate ward in a timely manner.
Top Tips for What to Do:
- Start sedation early:
As mentioned above, premedication prior to retrieval is vitally important. In most cases an antipsychotic (Olanzapine 10mg) and a benzodiazepine (Diazepam 10mg) is the premedication of choice. However, acute psychiatric patients presenting with drug induced psychosis (be it first or subsequent presentations) routinely require up to 20mg- 30mg of both Olanzapine and Diazepam orally. The first dose of sedation is given prior to the crew departing Darwin and then half an hour prior to the crews landing at the communities/ regional hospitals. This administration is overseen by the Medical Retrieval consultant (MRC) on duty. If the patient is not responding to the Olanzapine and Diazepam, the likelihood of requiring in-flight sedation is increased as is the probability of intubation for transport.
- In-Flight sedation:
We find in flight we tend to use midazolam, propofol and ketamine. The drug of choice is directly related to the flight doctor’s area of expertise. The ED Registrars tend to use midazolam and ketamine, whereas the ICU and Anaesthetic registrars head for the propofol and midazolam.
On arrival at the referral centre the patients are assessed for the need for further sedation prior to flight.
- Pre-Flight Sedation: Midazolam 2-5mg IV
- In-flight Sedation:
- Propofol Infusion 0.2-0.5mg/kg/hr and titrate as required
- Ketamine Infusion 0.5-1mg/kg/hr and titrate as required
A Richmond Agitation Sedation Scale (RASS) of -3 (Moderate) to -4 (Deep) or a Ramsey Sedation score of 5 indicates the level of sedation required for safe transport.
The ability to discontinue the sedative and allow the patient to wake prior to admission at the receiving centre is extremely important. If the flight crew are able to deliver an acute psychiatric patient to the receiving centre awake and ready for assessment this expedites the patients’ admission to the in-patient facility from the emergency department or, optimally allows for direct entry into the inpatient facility at the receiving centre.
Richmond Agitation Sedation Scale:
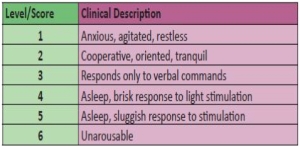
Ramsey Sedation Scale:
- Managing the environment:
Managing the stressors of flight is extremely important when retrieving an acute psychiatric patient. Using ear plugs, blankets to keep patients warm, positioning for comfort when heavily sedated, limiting cabin conversation and ensuring physical restraint are fastened appropriately ensures the acute psychiatric patient does not experience any extraneous stressors throughout their flight.
- Local law enforcement:
On occasion the local law enforcement will be involved with the acute psychiatric retrieval. The resource poor environment of the community clinic necessitates the presence of police to help control patients as documented under the section 9.
- Coordination:
The coordinating Medical Retrieval Consultant will liaise with the Consultant Psychiatrist on call at the hospital, alerting them to the impending admission. The Consultant Psychiatrist then coordinates with their in-patient team to ensure timely assessment of the patient if they are to be admitted through the emergency department.
Although the collective groan when another psychiatric retrieval arises resonates through the base we remain steadfast in our support to our rural and remote colleagues and we will continue to play a vital role in maintaining safety of the community, the families and the patients who are all touched by mental illness in the top end of the NT.